Our Research
Adipocyte-Derived Small Extracellular Vesicles as Mediators of Neurological Disease
Rachael Batabyal, M.D., Junior Investigator
We are experiencing concurrent epidemics of obesity and Alzheimer’s disease and related dementias (ADRD). ADRD is a progressive neurodegenerative disease that affects more than 5 million people in the United States. Patients with midlife obesity have a threefold increased risk of developing ADRD later in life; however, not all patients with obesity develop Alzheimer’s disease, and the mechanism relating obesity to the development of ADRD is poorly understood.
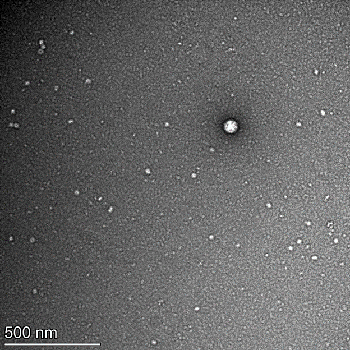
Our work explores adipocyte-derived small extracellular vesicles (ad-sEVs) as a possible mechanistic link between obesity and ADRD. Adipocytes release ad-sEVs which travel through the serum and carry microRNAs to distant organs. These microRNAs can then regulate gene expression in target organs. We are interested in how these ad-sEVs may travel across the blood-brain barrier and cause neurodegenerative diseases, such as ADRD.
The Role of Metabolism and Cellular Energetics in Sepsis
Ioannis Koutroulis, M.D., Junior Investigator
Our research focuses on sepsis metabolism. Sepsis is a very heterogeneous disease that may be involved in 20% of deaths worldwide. Multi-organ failure is responsible for the high mortality of sepsis but unfortunately, most treatments complementary to antibiotics and intravenous fluids have failed to show improved outcomes. Alterations in metabolism during the septic process, lead to decreased energy generation and immune cell dysfunction which has been implicated in organ failure. Our long-term goal is to identify novel therapeutic targets that can improve ATP production via aerobic cell respiration but also the host immune response. The focus on immunometabolism will allow us to define the role of cellular energetics in sepsis and other serious infections.
Maternal Adipocyte-Derived Exosomes in the Thin-Fat Indian Baby Paradox
We are currently working with collaborators in Pune and Bangalore, India to study the effects of maternal adipocyte-derived small extracellular vesical miRNAs on the developing fetus. India has the second-highest prevalence of diabetes in the world (71 million patients) and the largest number of low birthweight infants (6 to 8 million per year). At first glance, these data may seem unrelated. However, the association between birthweight and risk of diabetes as an adult is often described as “U-shaped,” meaning that both low- and high-birthweight babies have an increased risk of diabetes (as well as other noncommunicable diseases) as adults. While it iy fat. This is the so-called thin-fat paradox. These thin-fat infants, and their eventual offspring, have an extremely high risk of developing obesity and the subsequent sick fat (i.e., adiposopathy), which is likely at the root of obesity-associated, noncommunicable diseases. This has created an intergenerational spiral of non-communicable disease risk wherein maternal non-communicable diseases drive non-communicable disease risk in her offspring, and then the offspring, upon reaching childbearing ags not surprising that high birthweight infants have more adipose than normal-weight infants, low birthweight infants exhibit an even higher percentage of bode, pass this risk to the next generation.
Our work in the Freishtat Laboratory would propose a mechanism by which the health of the mother influences the health of the fetus, epigenetically, and may explain how these phenomena can be traced back to generational food insecurity. In particular, we are studying the influence of maternal obesity on adipogenesis and metabolism in the fetus via cross-placental transfer of maternal small extracellular vesicles. This work would further elucidate the complex communication between mother and fetus during development, and how maternal health affects long-term health of the child.
Examining Associations between Infant Bronchiolitis and Childhood Asthma
The largest cause of infant hospitalizations is bronchiolitis, which is a viral lower respiratory infection. Respiratory syncytial virus (RSV) and rhinovirus (RV) are the two main causes, but it can be caused by many other viruses. Symptoms of bronchiolitis may include typical flu-like symptoms and wheezing ranging from mild to severe. Not only are children acutely affected, but studies have linked being hospitalized for bronchiolitis with developing wheezing and asthma later in life. We are working with collaborators in Boston, Mass., to learn how to identify infants with bronchiolitis who are at a higher risk of developing wheezing or asthma. Our data show that the body reacts to RSV- and RV-induced bronchiolitis differently, as well as the body’s microbiome, which may contribute to severity of bronchiolitis and risk of later conditions.
Scientific Consortium for Non-Communicable Disease Reduction Across Generations (SCNR-G)
The world is facing a rapidly escalating epidemic of non-communicable diseases (NCDs), including obesity, diabetes, cardiovascular disease, cancer and neuropsychiatric illnesses. The burden of NCDs is astronomical and treatment is cost-prohibitive for even wealthy countries. This epidemic is associated with rapid socioeconomic and nutritional transitions experienced in both developed and low- and middle-income countries (LMIC) over the last 50 to 70 years. As this epidemic has developed over a minimum of two or three generations, intergenerational and early life (i.e., fetal and childhood) influences are strongly suspected to underlie its cause.
These early life influences underlie the developmental origins of health and disease (DOHaD) conceptual framework that describes how early life environments can impact the development of NCDs throughout the life span. Recent advances allow scientists to extend the DOHaD concept across multiple generations. Intergenerational effects of factors ranging from toxins to culture to genetics/epigenetics can now be explored. Yet research and development remain slow and siloed – rarely do NCD researchers look for causes in childhood, in utero, or in prior generations. A new model is needed to address the impact of NCDs. This model must break down traditional research/clinical siloes and geographic borders, to bring together teams with the expertise, resources, and patient cohorts needed, regardless of country and discipline of science.
The Scientific Consortium of Non-Communicable Disease Reduction Across Generations (SCNR-G, pronounced synergy) was formed in 2020 at Children’s National Hospital (CNH) in Washington, DC. This consortium will serve as a catalyst for international teams of clinicians and scientists to conduct DOHaD science and translate results to patients and families. To start, SCNR-G will consist of DOHaD research and clinical innovation programs in the United States of America (USA) and several other countries with interested scientists, clinicians and institutions. Countries involved in this first effort include India, Brazil, and the USA. With additional interdisciplinary relationships, the consortium will expand to the Middle East, European Union (EU) and Asia. Current collaborative DOHaD research programs in obesity, diabetes, and aging will be included as the initial foci.
Contact Us
For more information please contact us by email at info@scnr-g.org.
